Medical & Pharma
CT scans in COVID19 patients and the risk of cancer in future

- The COVID-19 pandemic posed an unparalleled challenge for the medical fraternity and created multiple challenges in the delivery of optimal care for patients, especially those with cancer, and the risks of exposure to frequent CT scans have increased the challenges even more.
- Despite extensive planning, the rapidly evolving and uncertain environment left patients and health care workers in uncharted waters.
- As COVID-19 spreads worldwide, there is a growing interest in the role and appropriateness of chest radiographs (CXR) and computed tomography (CT scan) for the screening, diagnosis, and management of patients with suspected or known COVID-19 infection.
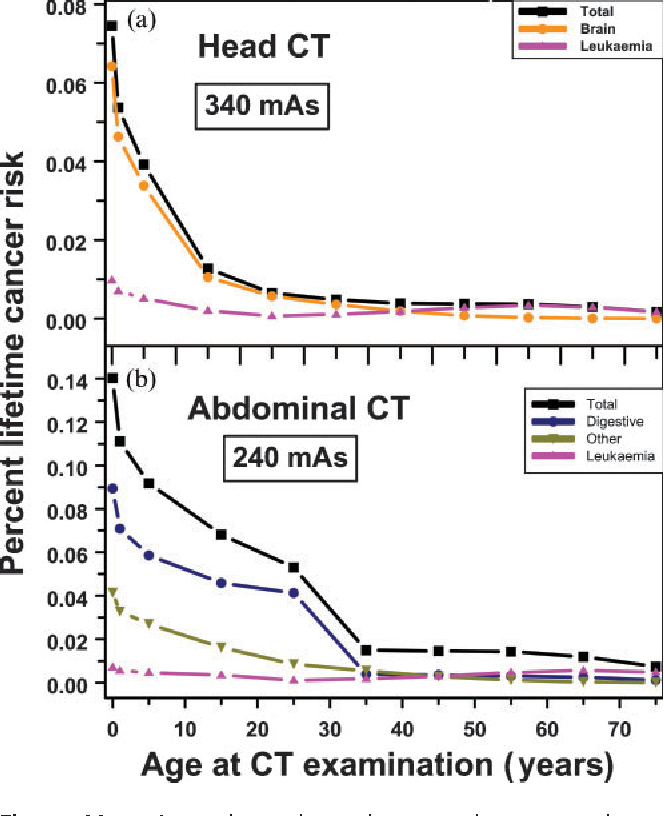
The advantage of these imaging modalities is their potential to spot patients who are highly suspicious of novel coronavirus-infected/pneumonia. The International Atomic Energy Commission has shown how CT scans at younger ages lead to greater cancer risk in later life. A CT scan is equal to 300-400 chest X-rays and we come across mild covid patients repeating CT scans every three days.

It’s highly not suggestable for oneself to expose to such harmful radiation. But due to scarcity of testing kits, many health centers have opted for the CT scan as a primary option to screen and determine the COVID-19 based on the CT-based scoring systems. Over a period, the screenings were recommended rampantly without much consideration about their long-term consequences such as radiation-induced adverse effects and its related cancers, both in patients and healthcare workers. At a point in time, their usage reached alarming levels, raising a huge debate among academicians, clinicians, and researchers.
In general, the radiation we get from x-ray, CT, and nuclear imaging is ionizing radiation – where high-energy wavelengths or particles will penetrate the tissues to reveal the body’s internal organs, and structures. There is a chance of such ionizing radiation damaging the DNA. Although cells in the human body repair most of the damage caused, they sometimes do the job imperfectly, leaving small areas of “misrepair.”
Increased risk of cancer from exposure to CT-scans
The result is DNA mutations that may contribute to cancer years down the road. Most of what we know about the risks of ionizing radiation comes from long-term studies of people who survived the 1945 atomic bomb blasts at Hiroshima and Nagasaki. These studies show a slightly but significantly increased risk of cancer in those exposed to the blasts, including a group of 25,000 Hiroshima survivors who received less than 50 mSv of radiation – an amount you might get from three or more CT scans.
Overall, the actual radiation exposure depends on many things, including the device itself, the duration of the scan, your size, and the sensitivity of the tissue being targeted. One chest CT scan delivers the amount in 100 to 200 X-rays. In a year, the average person gets about 3 millisieverts (mSv) and each CT scan delivers 1 to 10 mSv, depending on the dose of radiation and the part of your body that’s getting the test.
A low-dose chest CT scan is about 1.5 mSv and the same test at a regular dose is about 7 mSv. Overall, the odds are very low – the chance of getting fatal cancer from anyone’s CT scan is about 1 in 2,000. However, if the patient doesn’t have an option and have to undergo multiple scans in a short span, then he/she should discuss with their concerned clinician and ask their suggestion to consider for a lower dose scan (especially, it is highly recommended in cancer patients with a history of multiple scans performed in recent times).
A few tips to follow to minimize exposure from CT scans:
- Note down the date and type of scan underwent
- Discuss any high-dose diagnostic imaging with the clinician.
- Keep track of the x-ray history.
- Consider a lower-dose radiation test (write down the dose of radiation administered)
- Consider less frequent testing.
- Don’t seek out scans.

By Dr. Raj Nagarkar, CEO and Chief Surgical Oncologist, HCG Manavata Cancer Centre, Nashik, India