Medical & Pharma
Thalassemia – 3 Common Myths and Reality
- Thalassemia is one of the deadliest diseases.
- It is the most common inherited genetic blood disorder that affects the body’s ability to produce normal haemoglobin.
- People with thalassemia produce less healthy haemoglobin proteins and their bone marrow produces fewer healthy red blood cells. In India, about 10,000 children are born every year with thalassemia.
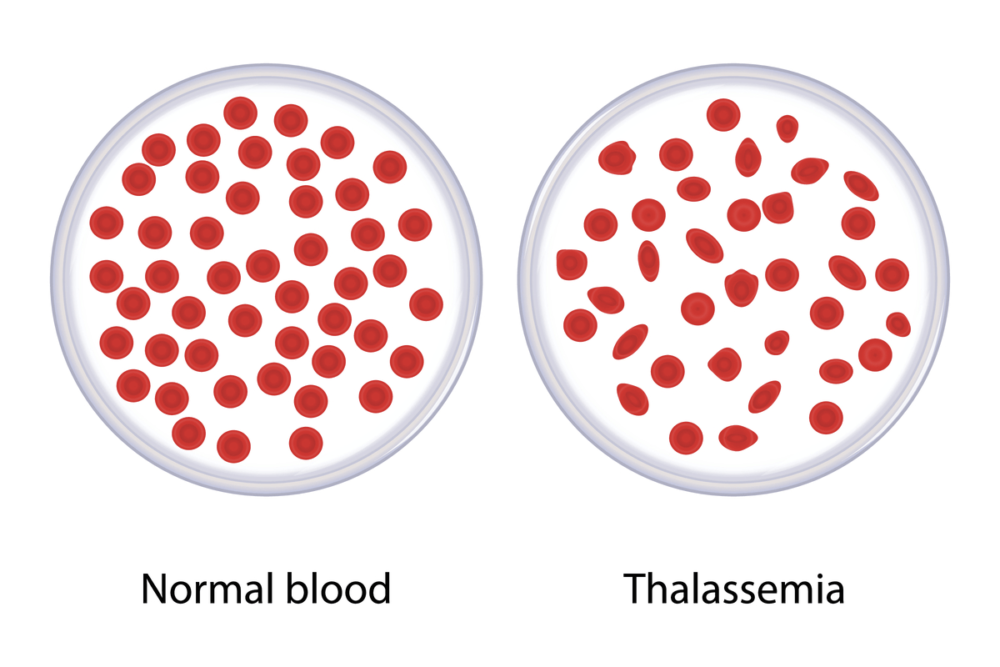
There are different types of thalassemia and the type of thalassemia a person may have depends upon the number of defective genes they have inherited.
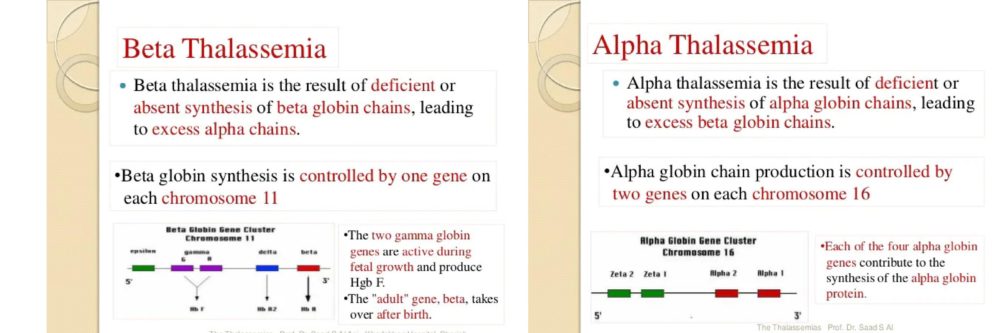
There are mainly 2 types of thalassemia:
- Beta-thalassemia – Major and Minor Subtype
- Alpha thalassemia – haemoglobin H and fetal hydrops subtypes.
2 types of Thalassemia
Thalassemia Major is found in children who receive mutated genes from their parents. The inherited child will be unable to produce the necessary haemoglobin, which eventually leads to chronic fatigue. People with thalassemia trait in one gene are Thalassemia Minor. The confirmation of Thalassemia Minor can happen through a specific blood test known as haemoglobin electrophoresis.
In transfusion-dependent, beta-thalassemia symptoms begin after a baby is few months old. In others, it can take few years. The symptoms can include:
- Pale skin
- Acting cranky or upset
- Not growing as much as expected
- Swelling of the belly
- The white part of the eyes turning yellow
- Facial bone or skull being wider than usual
- Dark urine
- Weakness
- Fatigue
Complications of Thalassemia
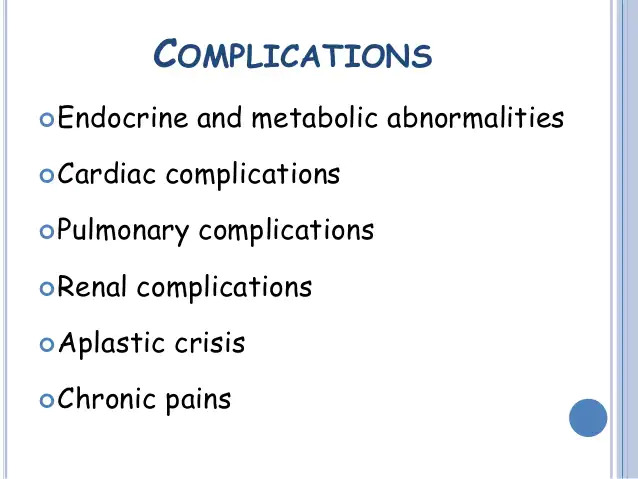
Complications of Thalassemia
Iron overload: Patients suffering from thalassemia can accumulate too much iron content in their bodies, either from the disease or from frequent blood transfusions. Excess iron may result in damage to the heart, liver, and endocrine system.
Infection: There are high chances of an increased risk of infection in a thalassemic particularly if the spleen is removed.
Heart-related issues: Associated with severe thalassemia are congestive heart failure and abnormal heart rhythms in patients.
Treatment Options of Thalassemia
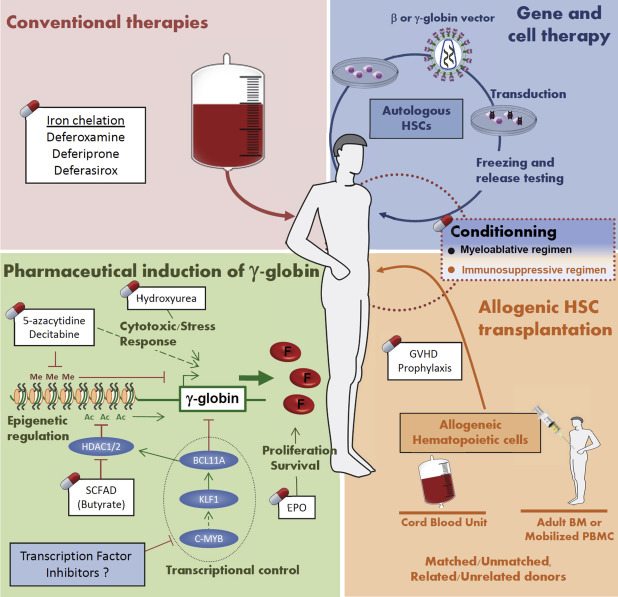
Treatment option includes blood transfusion and iron chelation versus transplantation for patients suffering from thalassemia. With a mild case, one might feel tired and not require treatment. But for serious cases, regular blood transfusions are required. How often one needs transfusions may vary from person to person.
Current and Future alternative treatments for Thalassemia
-
Transfusion and chelation therapy
Regular transfusion and chelation therapy have helped in improving the survival and quality of life of patients with thalassemia and have shifted a previously fatal disease with early death to a chronic disease that is compatible with prolonged survival. For effectiveness, treatment should start as early as the first few months after birth and should continue for life or until the patient undergoes transplantation.
-
Allogeneic Hematopoietic Stem Cell Transplantation (HSCT)
The realistic and clinically rationale curative modality available to treat thalassemia major is Allogeneic stem cell transplantation. Recent developments have advanced the technique from both siblings and alternate donors other thankfully matched siblings with different intensities of conditioning and graft engineering for global use.
There are multiple advantages of stem cell transplantation which includes
1. The high cure rate with the current advances in transplant engineering and conditioning regimens.
2. Lower cost and cost-effectiveness.
3. Improved impact on Quality of Life for both patients and families.
Here are the Myths that are important to be busted
Myth: Thalassemia carriers should not get married
Fact: People with thalassemia can get married to anyone. The couples must get their DNA testing done to see which mutation they have. However, if a thalassemia carrier marries a carrier, then at the time of 8-10 weeks of pregnancy, the expecting mother should go for antenatal diagnosis of thalassemia.
Myth: If two thalassemia carriers marry each other, they will have a thalassemia major child
Fact: One can also go for pre-implantation genetic testing to select the embryo that does not have the thalassemia gene along with a check for aneuploidy. This would ensure a non-thalassemia major birth despite both being thalassemia carriers.
Myth: There is no treatment for thalassemia major
Fact: If a thalassemia child is transfused with quality filtered blood regularly, the process can help the patient to get through to adulthood. Also, one must look at levels of ferritin for iron overload and oral iron chelation agents.
Ensure checking for early organ damage by performing an MRI of the heart, pancreas, and liver to get the best results for proper growth. The other options available for treatment are bone marrow transplants and gene therapy.
Thalassemia major patients should be offered transplantation before they develop end-organ damage and iron overload-related complications; the earlier the better. Thalassemia is certainly a dangerous disease, if detected at an early stage can be managed successfully with the help of timely preventive health check-ups.

By Dr. Suraj Chiraniya, Hemato Oncology and BMT, HCG Cancer Centre Mumbai.








































